Figure 13:
The fit of the titanium bar was tested in the maxillary bridge. Once the fit was confirmed, the gingival area and the anteriors were veneered with ICE Zirconia ceramic. In the anterior region, only vestibular ICE Zirconia dentines, effects and incisals were used; the incisal edge remained unveneered to avoid chipping. After stain and glaze firings, the restoration was complete.
Figure 11:
For a natural color, the restorations were brush-painted with acid-free Colour Liquids Prettau Aquarell; each stroke was manually applied with a thin brush and then the restorations were placed under a drying lamp. For visual aid, the liquids contain special bio-pigments that help in realistic shade distribution and color grading. Individual custom coloring of finer details such as mamelons, cervical or interproximal areas is considerably easier and can be performed with pinpoint precision.
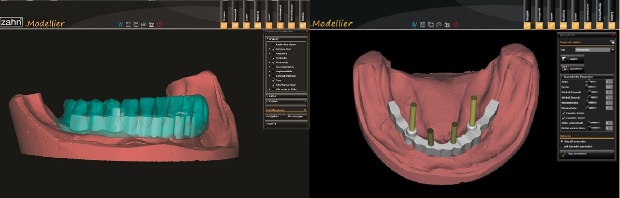
Figures 7 & 8:
The bar was scanned and the mandibular bridge designed on screen. To ensure adequate fit, function, esthetics and phonetics, temporary bridges were milled from Temp Basic resin (left photo) and veneered with gingival composites (right photo). The titanium bar and temporaries were sent to the dentist for the try-in
Figures 5 & 6:
Next, to determine the optimal position of the titanium support bar and define the emergence profile, the mandibular digital waxup was displayed on screen (left photo). The corresponding implant types in the software library were used to plan the bar construction that would be directly screw retained on the implants (right photo). The software stores all files as open .stl files, which can be easily exported.
The bar and connectors were then milled in titanium using the M5, a 5+1-axis simultaneous milling unit, and the bar was polished. Before designing the mandibular bridge, the fit of the milled titanium bar was examined on the master cast.
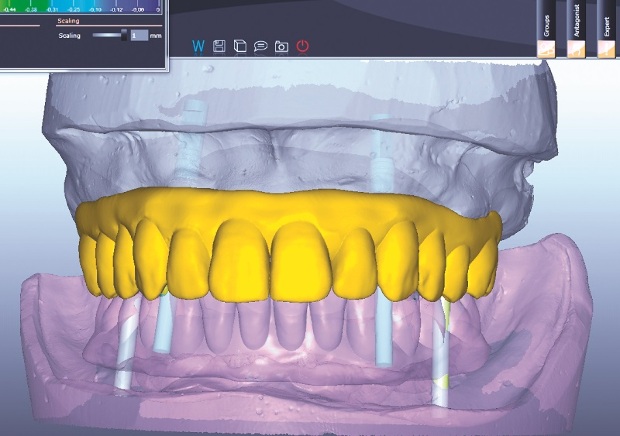
Figure 4:
A digital waxup of the maxillary bridge was created using the Zirkonzahn. Modellier software and its “Heroes Collection” tooth set library (the software also offers a wizard with step-by-step design instructions). The customized titanium bases were modified on screen to optimize the orientation of the screw-access channels. The software then analyzed the digital waxup situation and adapted it to the gingival and implant geometries.
Figure 3:
At the laboratory, the working casts were poured from the impressions, placed in the articulator and scanned using the fully automated, optical structured light scanner S600 ARTI. The software uses the articulator scan to determine the jaw relations and align the casts in perfect occlusion, allowing the identification and elimination of static and dynamic premature occlusal contacts.
Figure 2:
To support the maxillary bridge, four implants with titanium bases were placed at sites #4, #6, #11 and #13. The mandible (shown here) received implants at sites #20, #23, #26 and #28 and, since there were only four implants and an extensive distal edentulous space, the team decided to use a titanium bar to guarantee bridge stability.
The team was convinced that the esthetics and handling benefits of zirconia coupled with titanium’s high flexural strength would result in strong, esthetic and biocompatible restorations.
Figure 1:
The patient had conditionally removable dentures retained with metal clasps and wanted a more esthetic, fixed restoration. Her atrophied mandible presented a major challenge.
The dental team—including Drs. Fernando Rojas-Vizcaya and Homayoun Zadeh, and Georg Walcher, MDT—decided to restore her smile with eight implants, four upper and four lower, and fixed, metal-free suprastructures. Due to the limited bone available, the team chose occlusally screw-retained Prettau Bridges—fully anatomical restorations made with translucent Prettau Zirconia that are ideal for implant-supported restorations, limited-space situations and restorations with a gingival flange.